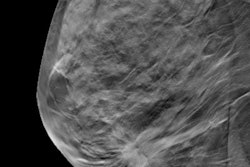
Adding screening digital breast tomosynthesis (DBT) to digital mammography reduces the number of women classified as BI-RADS 3 and, therefore, the number of women who are recommended for short-term follow-up, according to a study published in the November issue of Academic Radiology.
Since the BI-RADS 3 lesion classification recommends that women receive two years of follow-up performed at six-month intervals, reducing the number of referrals could have a significant positive effect, wrote a team led by Tricia Stepanek of Case Western Reserve University School of Medicine in Cleveland.
"This reduction of the number of women committed to short-term follow-up has the potential for downstream effects including decreased patient anxiety, improved patient outcomes, and decreased false-positive mammograms," the authors wrote. "In addition, the increased cost savings of avoiding follow-up diagnostic imaging is likely to outweigh the initial cost of DBT with screening."
The intention of the BI-RADS 3 category is to "reduce the number of unnecessary biopsies while maintaining an acceptable rate of cancer detection," Stepanek and colleagues noted. But the BI-RADS 3 category also brings challenges (Acad Radiol, November 2019, Vol. 26:11, pp. 1515-1525).
"Certain lesions may require repeat follow-up with both ultrasound and digital mammography, increasing the cost of the short-term follow-up approach," the group wrote. "Additionally, patient compliance is known to decrease with each consecutive follow-up. A reduction in BI-RADS category 3 use may result in both economic savings and improved patient outcomes."
Stepanek's team conducted a study that compared the use of BI-RADS category 3 in patients recalled from screening before and after DBT was implemented. The research included 11,478 digital mammography screening exams and 9,350 digital mammography plus DBT screening exams.
The researchers found that adding DBT to digital mammography screening decreased the number of lesions classified as BI-RADS 3 compared with screening digital mammography alone (2.4% versus 3.4%). Screening digital mammography plus DBT had a lower recall rate compared with digital mammography, at 11.8% versus 13%.
The team also found that delayed cancer detection rates for both groups exceeded the recommended 2% benchmark -- 2.3% for digital mammography and 3.6% for digital mammography plus DBT -- but when cases were limited to invasive cancers, these delayed cancer detection rates fell below the benchmark, at 1.5% for digital mammography and 0.9% for digital mammography plus DBT. Finally, the study showed a statistically significant reduction of 10.3 per 1,000 women designated for short-term follow-up.
The results suggest that adding DBT to digital mammography could improve patient outcomes as well as cut healthcare costs, according to Stepanek and colleagues.
The findings could "contribute to cost savings and a reduction in patient anxiety and time, potentially addressing some of the criticisms of mammography," they concluded.