Blastomycosis:
View cases of Blastomycosis
Clinical:
Blastomycosis (Blastomyces dermatitidis) is a thermally
dimorphic fungus endemic to the southeast/upper midwest U.S. along
the Ohio and Mississippi river (Great Lakes, Southeast/Mississippi
and South Central/Ohio River) and Canada, but is less common than
Histoplasmosis [5,6,7]. The fungus resides in moist soil in wooded
areas and inhaled spores result in primary lung infection [5].
Human to human spread of the disease does not occur [8]. Most
patients will have a subclincial disease course and will remain
asymptomatic [7]. The clinical presentation is variable and
patients who do present clinically typically develop symptoms
about 6 weeks following exposure [5,7]. Most patients with
symptomatic acute infection present with symptoms similar to
bacterial pneumonia (abrupt onset fever, chills, productive cough,
night sweats myalgia, and arthralgia [6,7]), but the infection
will usually resolve without treatment.
Hematogenous dissemination reportedly occurs less often than with
histoplasmosis [5]. Virtually any organ system can be involved and
multiorgan disease can be seen in 17-30% of patients [8]. The skin
is the most common extrathoracic site of involvement (20-70% of
cases), followed by bone (up to 25% of extrathoracic cases,
produces lytic lesions, and most commonly affects the vertebrae,
pelvis, skull, ribs, and long bones), the male genitourinary
system (prostatitis and epidiymo-orchitis), and the CNS (5-10% of
disseminated cases and most commonly produces epidural or
parenchymal abscesses followed by meningitis) [5,6].
Up to 50% of patients with cutaneous lesions have normal CXRs [8]. Skin manifestations include papules that progress to verrucous, plaque-like lesions with a sharp raised edge on exposed surfaces (that may contain pustules [7]) or mouth ulcers.
The infection is considered acute if patients have had symptoms
for under one month, and chronic if symptoms are present for a
longer period, or if nonpulmonary disease is present. Chronic
pulmonary symptoms occur more frequently than acute ones- with
intermittent low-grade fevers, mild persistent productive cough,
chest pain, hemoptysis and generalized symptoms may also be
present (malaise, fatigue, and weight loss) [5].
Because there are no reliable skin antigen or serological tests, the prevalence of asymptomatic disease is not known. Blastomycosis is found less often in immune compromised patients, probably due to the overall lower prevalence of the disease. However, diffuse disease and a higher mortality rate is seen in immunocompromised patients [5]. Fibrosing medistinitis has not been associated with Blastomycosis infection. Treatment initially consists of a one to two week period of observation for symptomatic patients. For those with progressive disease, ketoconazole or amphotericin B therapy can be instituted with cure rates of up to 89% and 97%, respectively. In a small percentage of cases, blastomycosis has a fulminant course with fevers, chills, shortness of breath, rapid systemic dissemination, and ARDS within one week (often leading to death) [5].
X-ray:
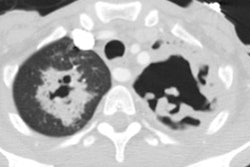
The radiographic findings of acute disease are airspace
consolidation (up to 75% of cases) with patchy, ill-defined
opacities with airbronchograms and an upper lobe predilection
(lobar consolidation is uncommon) [5,8]. Focal masses are the
second most common radiographic finding (up to 30% and can mimic a
malignancy) [5] (other authors indicate that masses are the most
common feature and are seen in 88% of patients [6]). The masses
are usually well circumscribed and between 3-10 cm in diameter
with a paramediastinal or perihilar distribution [5].
Reticulonodular interstitial disease (6-9% of cases and this
usually produces a tree-in-bud appearance on CT), and nodular or
miliary patterns (11-28% of cases and more common in
immunocompromised patients) have also been described. Cavitary
disease is uncommon (15% of cases).
Hilar and mediastinal adenopathy are uncommon (probably less than
10% of cases), but other authors suggest adenopathy can be seen in
25% of infected patients [8]. Pleural effusion occurs in 5-20% of
cases) and usually small when seen [5,6].
There is little correlation between the radiographic findings and the clinical symptoms. Unlike in histoplasmosis, pulmonary nodules and lymph nodes typically do not calcify [8].
REFERENCES:
(1) Semin Roentgenol 1996; Jan 31(1):45-51
(2) ACR Syllabus #40: p. 171-173
(3) J Thorac Imag 1999; Conces DJ. Endemic fungal pneumonia in immunocompromised patients. 14: 1-8
(4) Radiol Clin N Am 2005; Tarver RD, et al. Radiology of community-acquired pneumonia. 43: 497-512
(5) Radiographics 2007; Fang W, et al. Imaging manifestations of
blastomycosis: a pulmonary infection with potential dissemination.
27: 641-655
(6) Radiographics 2011; Kanne JP, et al. Beyond skin deep:
thoracic manifestations of systemic disorders affecting the skin.
31: 1651-1668
(7) Radiology 2016; Mouser H, et al. Case 233: Blastomycosis.
280: 972-977
(8) Radiographics 2021; Kunin JR, et al. Thoracic endemic fungi in the United States: importance of patient location. 41: 380-398