Mediastinitis:
View cases of mediastinitis
Clinical:
Most cases of acute mediastinitis are secondary to postoperative
complications and esophageal perforation [5]. Acute sternal
osteomyelitis and septic arthritis of the sterno-clavicular joint
may spread into the mediastinum [5]. Risk factors for sternal
osteomyelitis include IV drug use, HIV, and other immunodeficiency
conditions [5]. Risk factors for sterno-clavicular septic
arthritis (most commonly S. aureus or P. aeruginosa) include
diabetes, rheumatoid arthritis, and IV drug use [5]. Despite
appropriate antibiotic therapy and surgical removal of infected
and necrotic tissue/debridement relapse occur in up to 18% of
patients with staphylococcal mediastinitis [6].
Mediastinitis is a relatively uncommon (incidence 0.5 to 5%), but
serious complication following median sternotomy (mortality 7-80%)
[5]. Mortality can be decreased if the diagnosis is made early and
sternal debridment and antibiotic lavage are performed [1]. The
most common organism for post-op mediastinitis is S. aureus [5]. Risk factors
include diabetes, obesity, internal mammary artery harvest,
excessive cautery, and prolonged surgical duration [7]. Symptoms
include fever, eryhtema, surgical site drainage, chest pain,
sternal instability, and sternal dehiscence [7].
Normal post-surgical findings after sternotomy include callus
formation (which begins after the 3rd post-op month), small gaps
or offsets, and impactions [4]. Only 50% of sternotomies appear
completely healed after 6 months; however, sternal union should be
complete within one year of the procedure [4].
Dehiscence- which is defined as identifiable disruption of the
sternotomy- is frequently associated with the development of
mediastinitis [4,5]. The development of dehiscence later than the
2nd week after sternotomy is suggestive of mediastinitis [4].
Clinically patients present with acute chest pain, high fever,
chills, and leukocytosis [5]. Obesity, insulin-dependent
diabetes,and the use of internal mammary artery grafts (especially
bilateral grafts) are risk factors for the development of
postoperative mediastinitis [5].
X-ray:
CXR: Radiographic abnormalities frequently precede the clinical diagnosis of sternal dehiscence by an average of 3 days [4]. On plain film radiographs, sternal wire migration or rotation is an indication that the patient has developed a sternal dehiscence which may be secondary to mediastinitis [4]. Occasionally, a mid-sternal vertical lucency wider than 3 mm can be seen representing the separating fragments [4]. Gaps less than 3 mm are usually not associated with clinical instability, but progressive widening of the incisional gap is indicative of dehiscence [4]. Other findings of mediastinitis include mediastinal widening and loss of the normal mediastinal contour [5]. Air-fluid levels may be seen within the anterioir mediastinum on the lateral view.
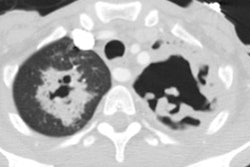
Computed tomography: Following mediansternotomy strandy densities can be seen within the anterior mediastinal fat for up to 2 to 3 weeks, however, the mediastinal fat planes are generally preserved. Small collections of air may be identified normally for up to 7 days after the procedure. Focal retrosternal fluid collections or hematomas may also be identified for several days to 2 weeks- again, the mediastinal fat planes are usually preserved. The sternal defect may be slightly irregular or offset. A small amount of pericardial thickening or fluid can be expected in the early post-operative period.
Similar to CXR, a lucent separation between the sternal fragments
of mor than 3mm is suggestive of dehiscense [5]. Findings of
mediastinitis include localized mediastinal fluid collections and
the presence of mediastinal air. Secondary findings include
edema/increased density within the adjacent mediastinal soft
tissues (with obliteration of the mediastinal fat planes [3]),
sternal separation, pleural effusion, and adenopathy. Early
sternal osteomyelitis can be very difficult to differentiate from
normal post-surgical sternal irregularities.The presence of
mediastinal gas bubbles and fluid collections after the 14th
post-operative day is has a sensitivity and specificity
approaching 100% for acute mediastinitis [5].
In the early post-operative period (to day 14 post-op), normal post-operative changes within the mediastinum (as discussed above) may mimic mediastinitis- during this period, CT scan has a specificity of as low as 33%. Significant improvement in specificity occurs after day 14 (up to 100% in one article). The sensitivity remains high (up to 100%) both in the early and late post-operative periods. Despite its low specificity, CT can still prove useful in guiding aspiration and drainage of fluid collections which can then be sent for culture. [1,2]
REFERENCES:
(1) AJR 1992; Templeton PA, Fishman EK. CT evaluation of poststernotomy complications.159; 45-50 (Review. No abstract available)
(2) Radiology 1996; 201: 463-466
(3) AJR 2003; Li AE, Fishman EK. Evaluation of complications after sternotomy using single- and multidetector CT with three-dimensional volume rendering. 181: 1065-1070
(4) Radiographics 2009; Restrepo CS, et al. Imaging
appearances of the sternum and sternoclavicular joints. 29:
839-859
(5) Radiographics 2011; Katabathina VS, et al. Nonvascular,
nontraumatic mediastinal emergencies in adults: a comprehensive
review of imaging findings. 31: 1141-1160
(6) J Nucl Cardiol 2015; Rouzet F, et al. Diagnostic value of
99mTc-HMPAO-labeled leukocytes scinitgraphy in suspicion of
post-sternotomy mediastinitis relapse. 22: 123-129
(7) AJR 2018; Hota P, et al. Poststernotomy complications: a multimodality review of normal and abnormal post operative imaging findings. 211: 1194-1205