Septic Pulmonary Emboli:
Clinical:
Septic pulmonary emboli are seen most commonly in IV drug users
(associated with
tricuspid valve endocarditis), immunocompromised patients with
infected
indwelling catheters, and in patients with periodontal disease
[3].
Typically patients present with fever, cough, and hemoptysis. In
patients with septic emboli from endocarditis and bacteremia, the
mortality rate can be between 4% to 26% [4].
X-ray:
Radiographs characteristically demonstrate multiple poorly
marginated 1 to 3 cm nodules or peripheral wedge-shaped opacities
that can cavitate with moderately thick walls, but patchy areas of
air-space consolidation may obscure the nodules. Pleural effusions
are
common. CT is superior to CXR in showing the presence and extent
of
septic emboli [3].
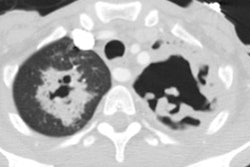
On CT, the most characteristic finding are multiple
pulmonary nodules in varying stages of cavitation and sub-pleural
wedge-shaped infiltrates (70-75% of patients). The pulmonary
nodules often have definable "feeding vessel" (60-70% of patients)
associated with them. However, on multi-planar reconstruction
images,
these vessels may actually course around the nodule [3]. A reverse
halo sign- a focal rounded area of ground glass opacity surrounded
by a more or less complete ring of consolidation- can be seen [4].
REFERENCES:
(1) AJR 2000; Rossi SE, et al. Nonthrombotic pulmonary emboli. 174: 1499-1508
(2) Radiographics 2003; Han D, et al. Thrombotic and nonthrombotic pulmonary arterial embolism: spectrum of imaging findings. 23: 1521-1539
(3) AJR 2006; Dodd JD, et al. High-resolution MDCT of pulmonary
septic embolism: evaluation of the feeding vessel sign. 187:
623-629
(4) AJR 2013; Nemec SF, et al. Lower lobe-predominant diseases of
the lung. 200: 712-728
(5) AJR 2020; Almeida RR, et al. Frequency and reliability of the
reverse halo sign in patients with septic pulmonary embolism due
to IV substance use disorder. 214: 59-67