Cytomegalovirus (CMV):
Clinical:
CMV is a DNA virus of the herpes group [5]. CMV can remain dormant within a host cell for years and be reactivated when host immune defenses are depressed [5].In immune competent patients, the infection is usually asymptomatic or produces mild flu-like symptoms [7]. CMV is the most common viral pathogen to cause significant significant morbidity and mortality in AIDS patients [2]. At autopsy, up to 80% of AIDS patients have evidence of CMV infection [2]. None-the-less, CMV is not a common cause of clinical pneumonia in these patients [3]. CMV infection often co-exists with other infections such as PCP and it is usually not the cause of clinical pulmonary disease. Recent studies, however, suggest an increase in CMV pneumonitis in HIV patients- likely related to advanced life expectancy and greater levels of immune compromise [2]. Affected HIV patients typically have very low CD4 counts below 50-100 cells/uL. Extra-thoracic CMV infection can be found in up to two-thirds of HIV patients with CMV pneumonia [2,3].
Despite it's occurrence in HIV patients, CMV pneumonia is more
commonly
seen in organ or bone
marrow
transplant patients being treated with cyclosporin and it is
one of
the most common causes of life-threatening opportunistic pulmonary
infection in those patients [4]. CMV pneumonia occurs in 10-40%
(up to
70% [6]) of bone marrow recipients and it usually results from
reactivation of a previously latent infection [4] (these patients
are
usually asymptomatic
[3]). The infections typically occurs during the post-engraftment
period 30-100 days following transplant [4], with a median onset
time
of 50-60 days after transplantation [6]. CMV infection can also
occur in solid organ transplant patients, and lung and small
intestine transplant patients are at the highest risk (possibly
related to the intensity of immunosuppression and the amount of
lymphoid tissue in the transplanted organs) [7].
Clinically patients present with fever, non-productive cough, dyspnea, and hypoxemia [4]. Mortality from CMV pneumonia in organ transplant patients remains high (20 to 40%) [3].
There is no clinical consensus regarding an acceptably sensitive and timely means for the early diagnosis of CMV pneumonia. Positive viral cultures from BAL fluid do not necessarily confirm infection [2]. The identification of intranuclear inclusion bodies on BAL or transbronchial biopsy is generally considered necessary for the diagnosis [2]. Establishing the diagnosis is critical because the infection responds to antiviral therapy. Treatment for CMV infection is gancyclovir or foscarnet.
X-ray:
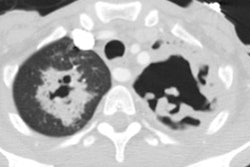
Radiographic findings vary widely from normal to airspace consolidation (in 65% of cases), to ground glass attenuation, to interstitial reticulation.On HRCT, ill-defined ground-glass attenuation is usually seen [5]. Discrete centrilobular pulmonary nodules have been described on HRCT (particularly in non-AIDS patients), as has airway disease with bronchial and bronchiolar wall thickening.
In HIV patients, airspace disease is the most common finding
(about
85% of cases) and it is characterized by areas of bilateral
asymmetric ground glass
attenuation,
dense consolidations, or a mixed pattern. Interstitial disease is
less
common (14% of cases). Other findings such as centrilobular
nodules (up
to 2 cm), bronchiectasis, and bronchiolitis (centrilobular
branching
densities)
have also been described.Thickened interlobular septa are also
observed [7].
(1) Curr Opin Pulm Med 1997; 3: 151-158
(2) Radiologic Clinics of North America 1997; McGuinness G. Changing trends in the pulmonary manifestations of AIDS. 35 (5): 1029-1082
(3) J Thorac Imaging 1999; McGuinness G. Viral and pneumocystis infections of the lung in the immunocompromised host. 14: 25-36
(4) AJR 2003; Franquet T, et al. Thin-section CT findings in 32 immunocompromised patients with cytomegalovirus pneumonia who do not have AIDS. 181: 1059-1063
(5) AJR 2005; Miller WT, Shah RM. Isolated diffuse ground-glass
opacity in thoracic CT: causes and clinical presentations. 184:
613-622
(6) Radiology 2011; Franquet T. Imaging of pulmonary viral
pneumonia. 260: 18-39
(7) Radiographics 2018; Koo HJ, et al. Radiographic and CT features pf viral pneumonia. 38: 719-739