Candidiasis:
Clinical:
Pulmonary candidiasis is a relatively common complication in the immune compromised, particularly in patients with hematologic malignancies such as leukemia and lymphoma. About half of the affected patients have a prior or concurrent bacterial infection which results in tissue damage, about 50% are receiving parenteral nutrition, and nearly 90% are receiving broad spectrum antibiotics. Patients generally present with pneumonia, and deteriorating liver and renal function. Discrete, nontender, firm, raised, red-pink, non-blanching characteristic skin lesions are discovered in only 10% of cases. Other patients at risk for infection include patients with chemotherapy induced neutropenia, stem cell transplant patients, IV drug users, and HIV patients [3].X-ray:
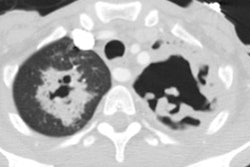
The radiographic appearance is non-specific, consisting of patchy, bilateral air space consolidations, or occasionally a diffuse miliary pattern (usually associated with hematogenous dissemination from the GI tract). Pleural effusions occur in up to 25% of cases. Adenopathy and cavitation is uncommon. On HRCT there is predominantly a nodular pattern. Halos of ground-glass surrounding the nodules can be seen in up to 60% of cases. Frank areas of consolidation or ground-glass attenuation have also been described.REFERENCES:
(1) Semin Roentgenol 1996; Imaging in candidiasis. 31(1), 76-82 (no abstract available)
(2) J Thorac Imaging 1999; Connolly JE, et al. Opportunistic fungal pneumonia. 14: 51-62
(3) Radiology 2005; Franquet T, et al. Pulmonary candidiasis after hematopoietic stem cell transplantation: thin-section CT findings. 236: 332-337