Hydatid Disease:
Clinical:
Hydatid disease is caused by infection by the tapeworm Echinococcus
granulosis or E. multilocularis (man ingests
the ova and becomes the intermediate host). Infection results in
primarily
hepatic disease, and only rarely involves the thorax. However, the
lung is the second
most common site of infection (the liver is the most common) and
pulmonary infection develops in 10% to 30% of all patients [3].
The right lung is affected in 60% of cases (likely due to greater
risk for trans-diaphragmatic spread from the liver) and 20% of
cases are bilateral [3]. Synchronous hepatic involvement is seen
at the time of diagnosis in only 20-40% of patients [3].
Patients
are generally asymptomatic, but may present with cough (53-62%),
dyspnea (10-70%), hemoptysis (12-21%), bilioptysis, pneumothorax,
paracystic pulmonary embolism, or anaphylaxis secondary to cyst
rupture [2].
Pulmonary cysts may rupture into the bronchus and the patient
will present with a complaint of "coughing up grape skins
(which are the cyst walls)." The infection can be diagnosed
by the use of an immunologic serum test, but the test is positive
in only 50% of patients with isolated lung disease.
Treatment is surgical removal without spilling the contents of the cyst. If the cyst cannot be excised safely, it should be sterilized by instillation of 10% formalin, 1% iodine, and 0.5% silver nitrate prior to drainage. Drainage procedures are often combined with mebendazole, albendazole, or praziquantel therapy.
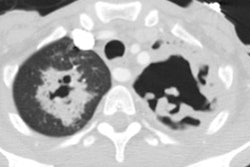
X-ray:
CXR may demonstrate the presence of one or multiple (30-60%), unilateral or bilateral (20-50%) rounded, nodules in the lung (normally the cysts are fluid filled). About 50-60% of the lesions are found in the lower lobes [3]. The nodules can range in size from 1 to 20 cm [2]. If rupture into a bronchus occurs, a crescentic layer of air can be seen above the collapsed cyst membrane floating within the cyst (meniscus or crescent sign) [2]. About 50% of patients are noted to have air-fluid layers within the cyst when they first present for medical attention. Cyst wall calcification can occur late, but is much less common (0.7% of cases) than calcification of the hepatic cysts.
REFERENCES:
(1) Radiographics 2000; Pedrosa I, et al. Hydatid disease: Radiologic and pathologic features and complications. 20: 795-817
(2) Radiographics 2005; Martinez S, et al. Thoracic manifestations
of tropical parasitic infections: a pictoral review. 25: 135-155
(3) Radiographics 2017; Zalaquett E, et al. Imaging if hydatid disease with a focus on extrahepatic involvement. 37: 901-923