Schistosomiasis:
Clinical:
Schistosomiasis is a helminthic infection endemic to tropical and subtropical regions in Africa, South America, Asia, the Middle East, and the Caribbean [2]. Human infection occurs through direct contact in fresh water [2]. The organism penetrates the skin, migrates to the dermal veins, and eventually to the pulmonary vasculature [2]. From the lungs, the organism travels via the systemic circulation to the liver where it resides in the portal venous system of the liver [2]. The infection can be divided into 3 categories- allergic dermatitis, acute schistosomiasis, and chronic shistosomiasis [3]. Acute schistosomiasis can be seen in primary exposure of individuals traveling in endemic regions [2]. The clinical presentation of acute disease is very variable, but most patients are asymptomatic [2]. Katayama fever (an acute febrile episode) may be seen 3-8 weeks after the initial infection and is due to a immunogenic/hypersensitivity response to the eggs released by the organism [2]. Katayama syndrome occurs as the organism passes through the lungs and the findings include an acute febrile illness with eosinophilia and diffuse pulmonary nodules (2-15 mm) or patchy interstitial or alveolar infiltrates [1,3].
Other findings include chills, arthralgia, nausea, headache, diarrhea, hepatosplenomegaly, and eosinophilia [2]. Pulmonary disease is more commonly associated with S. mansoni or japonicum infection. Patients can present with cough and wheezing [2]. Nearly one-third of patients with clinical schistosomiasis have pulmonary involvement. Clinical resolution is rapid without therapy, but infiltrates may worsen. Treatment is with Praziquantel.
In the chronic form of infection, embolization of ova to the small arteries in the lungs results in multiple pseudotubercles and the granulomatous reaction about the eggs results in obliteration of the vascular lumen [1,2]. Ultimately, this process results in intimal fibrosis and pulmonary arterial hypertension [1,2].
X-ray:
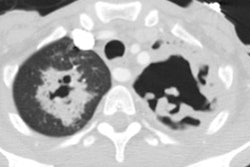
CXR findings are typically ill-defined nodules [2]. On CT, the most common finding is pulmonary nodules ranging in size from 2-15 mm, they can be well- or poorly defined, and a ground-glass halo about the nodule can be seen [2].
REFERENCES:
(1) Radiographics 2005; Martinez S, et al. Thoracic manifestations of tropical parasitic infections: a pictoral review. 25: 135-155
(2) AJR 2006; Nguyen LQ, et al. Acute schistosomiasis in nonimmune travelers: chest CT findings in 10 patients. 186: 1300-1303
(3) Radiographics 2007; Jeong YJ, et al. Eosinophilic lung diseases: a clinical, radiologic, and pathologic overview. 27: 617-639