Histoplasmosis:
View cases of Histoplasmosi and Fibrosing Mediastinitis
Clinical:
Histoplasmosis is a dimorphic fungus most commonly found in soil along river valleys. The organism is endemic to the Ohio and Mississippi river valleys. Bird or bat droppings are the media for its growth. The organism exists as mycelia in the environment and is inhaled into the lungs where it reaches the alveoli. Once at body temperature the organism converts to the more familiar yeast phase. In the normal host the yeast organisms are engulfed by macrophages where they proliferate until the host develops specific cellular immunity and delayed hypersensitivity which requires 12-14 days. During the interval the infected macrophages migrate to regional lymph nodes where there is commonly dissemination to the reticulo-endothelial system. Once delayed hypersensitivity develops the infection is controlled. Eventually there is calcification at the initial site of infection and within the involved lymph nodes [12]. There are 3 forms of infection:
1- Primary Disease:
The vast majority of individuals with normal immunity who develop
histoplasmosis experience a clinically unrecognized infection
(99.5% of cases [17]). Chest radiographs in these patients are
usually performed at some point after the infection, and the most
frequently encountered abnormality is a solitary, well marginated,
pulmonary nodule. Symptomatic patients develop a benign, self
limited illness characterized by mild, generally non-productive
cough to flu-like symptoms.
The CXR is normal in 40 to 70% of cases. In symptomatic patients the most common radiographic finding is a single area or multiple patchy areas of consolidation and adenopathy which can progress to form a solitary or multiple pulmonary nodule(s) (histoplasmoma). A miliary pattern can be seen. The lesions heal with calcification (granulomas). Some nodules may continue to slowly enlarge (doubling time 14-113 months) because of continued elaboration of collagen at the peripheral of the lesion- possibly a response to leakage of H. capsulatum antigen [12]..
Immune compromised patients are still at risk for H. capsulatum infection. The CXR may be normal in up to 50% of cases. The most common radiographic finding is a diffuse miliary pattern. HRCT will also demonstrate a diffuse pattern of 1 to 3 mm nodules and there is frequently associated hilar or mediastinal adenopathy [2].
2- Chronic Pulmonary Histoplasmosis:
Chronic disease occurs almost entirely in patients with pre-existing COPD. Patients complain of malaise, cough, and night sweats [12]. Spores are deposited within bullae where they stimulate the development of fluid within the cavity. The disease generally involves the upper lobes (apical-posterior segments). Segmental airspace opacities are seen and abut the pleural surface. Cavitation (similar to TB) with considerable fibrosis is seen as the disease progresses.
3- Disseminated Disease:
Disseminated histoplasmosis is a systemic illness that affects multiple organ systems and occurs in about 0.5% of cases [17]. It occurs in immunocompromised/immunosuppressed patients with defective T-cell immunity (due to lymphoreticular malignancy, cytotoxic agents, corticosteroids, or HIV). Patients at the extremes of age are also at risk for disseminated disease [11]. Symptoms include fever, weight loss, cough, and dyspnea. The infection may represent progression of a primary histoplasmosis infection or reactivation of a previously dormant infection [1]. Patients can develop a raised skin lesion, lytic bony lesions, hepatosplenomegaly (hepatic involvement is seen in 90% of cases [15]), peripheral lymphadenopathy, or epididymitis/prostatitis. A normal CXR is seen in about 30% of non-HIV immune compromised patients. Diffuse, small (under 3mm), nodular opacities are the most common radiographic feature. Linear and irregular opacities are the next most common finding. Focal air space opacity is seen infrequently (about 10% of cases) and adenopathy is rare [11]. The adrenals are also involved in a majority of cases [12].
4- Histoplasmosis in HIV:
Histoplasmosis occurs in about 2-5% of AIDS patients [10]. Patients typically have severe immune suppression (CD4 below 100 cells/uL) and nearly 75% of affected patients have disseminated disease [10]. Approximately one-third of HIV patients with disseminated histoplasmosis will have a concurrent opportunistic infection at the time of diagnosis [1]. Plain film radiographic findings are varied and non-specific. The chest radiograph can also be normal in up to 40-50% of cases. Nodular opacities are the most common finding typically diffuse, small (under 3 mm) nodular opacities [1]. Diffuse linear or irregular opacities are the next most common finding [1]. Focal air space opacities are found in only 10% of cases [1]. Pleural effusions and adenopathy are infrequently encountered [1].
Complications of Hisplasmosis Infection:
1- Broncholithiasis:
Calcified lymph nodes erode through the bronchial wall and produce obstruction. Patients typically present with post-obstructive pneumonia. It is important to remember that broncholithiasis is not associated with a soft-tissue mass- if one is identified, another etiology should be considered.
2- Mediastinal Granuloma:
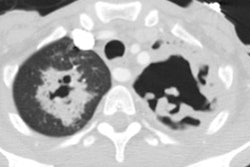
A mediastinal granuloma is a large mass of mediastinal lymph nodes that have become matted together and broken down into a single mass encapsulated by a thin fibrous capsule and there is no local invasion or associated mediastinal fibrosis [13]. It is an uncommon late sequella of mediastinal adenitis [3]. Some authors feel that mediastinal granuloma is the precursor of fibrosing mediastinitis [8], while others consider the two lesions as completely separate clinical entities [3]. Although a mediastinal granuloma may produce compression of mediastinal structures as a result of its size, there should be no associated fibrotic reaction [4]. Treatment with steroids to decrease the risk of progression to mediastinal fibrosis is not beneficial [8] and surgical resection is controversial [3,13]. The lesion is most frequently found in the right paratracheal region. Affected patients are usually asymptomatic. On CT, the lesion appears as a low density soft tissue mass which contains enhancing septae.
3- Fibrosing Mediastinitis:
Fibrosing (sclerosing) mediastinitis or idiopathic fibroinflammatory lesion of the mediastinum [13] is an uncommon late sequella of mediastinal adenitis. It occurs most commonly as a complication of histoplasmosis infection. Other less common infectious etiologies associated with the disorder include prior TB, actinomycosis, aspergillosis, blastomycosis, or cryptococcus infection. In addition, fibrosing mediastinitis can occur in association with other idiopathic fibrotic disorders such as retroperitoneal fibrosis, orbital pseudotumor, Reidal struma, sclerosing cholangitis, and methylsergide therapy. Fibrosing mediastinitis has also been reported in the setting of autoimmune disease, Behcet disease, rheumatic fever, radiation therapy, trauma, and Hodgkins disease [13].
In cases in which the disorder is associated with prior Histoplasmosis infection, it is postulated to occur as a result of leakage of antigen from casseous nodes into the mediastinum which stimulates an abnormal immunologic/inflammatory reaction that ultimately results in fibrosis [13]. Evidence of active infection (ie: the presence of Histoplasma organisms) is not found in this condition [6]. The fibrous infiltration of the mediastinum may constrict or obstruct mediastinal structures such as the SVC, pulmonary arteries or veins, the bronchi or trachea, and the esophagus. Two radiographic patterns have been described [4,13]:
1- A localized/granulomatous form: This is the most common
manifestation- 80-90% of cases [16]. The lesion occurs most
commonly in the right paratracheal or subcarinal region and the
mass frequently contains stippled calcification [13]. This form is
strongly associated with prior Histoplasmosis infection and is
felt to be related to an abnormal immunologic response to H.
capsulatum antigen with resultant proliferation of
fibro-inflammatory tissue in the mediastinum [16]. Affected
patients are typically between the ages of 35-46 years, but a wide
age range has been reported and there is no sex predilection [16].
Rarely, the condition can also occur in association with other
infections such as TB, other fungal infections (blasto,
mucormycosis, or cryptococcus), and inflammatory conditions such
as sarcoidosis [16]. The most frequently affected areas are the
right paratracheal region, the subcarinal region, and the hila
[16].
2- A diffuse infiltrative form: This form accounts for about
10-20% of cases. The lesion diffusely infiltrates multiple
mediastinal compartments and does not contain calcification. This
form is commonly idiopathic or associated with other
fibroinflammatory conditions (including IgG4 related disease),
drugs (such as methysergide), or prior radiation [13,16], but can
also be seen with prior Histoplasmosis infection. Affected
patients are typically middle aged or elderly and more commonly
men [16].
Affected patients are usually young and can be asymptomatic. Symptoms develop as the process gradually encases and obliterates vital mediastinal structures. Symptoms include cough, dyspnea, superior vena caval syndrome, hemoptysis (27-31%- which can be massive), chest pain, lithoptysis, and hoarseness. Pulmonary venous occlusion can result in progressive or exertional dyspnea, as well as hemoptysis [13]. This pattern of symptoms has been called "pseudo-mitral stenosis syndrome" [13]. Pulmonary venous occlusion can also lead to pulmonary infarction [13]. Pulmonary arterial stenosis or occlusion can less commonly result in pulmonary hypertension [13]. The esophagus is infrequently involved, but involvement can result in dysphagia. Males and females are affected equally [13]. The condition can be progressive with death as a result of cor pulmonale or relentless respiratory compromise
Treatment options include systemic antifungal or corticosteroid
therapy, surgical resection, or local therapy for complications
[13]. Limited data suggest that ketoconazole therapy may result in
disease stabilization, but controlled studies are not available to
confirm this benefit [13]. Other authors suggest that there is
insufficient data to support the use of antifungal agents and
conventional inflammatory drugs in patients with the
localize/granulomatous form [16].
Treatment with steroids may be of some benefit in patients with the idiopathic variety of the disorder, but are not likely to improve outcome in patients with fibrosing mediastinitis as a result of prior Histoplasmosis [4]. Surgical intervention can be performed to relieve vascular or bronchial obstruction, and for cases of significant hemoptysis. Extensive vascular or airway reconstruction may be required [13]. Bilateral mediastinal involvement generally precludes a surgical approach [13]. On the whole, the results of surgical therapy have been disappointing and resection is often associated with high morbidity and mortality [13]. Local therapies (with stents or balloon dilatation) are now used with increased frequency with efforts directed towards reopening occluded or stenosed airways [13].
CXR: The chest radiograph may appear normal, reveal a non-specific widening of the mediastinum, or may demonstrate the presence of a lobulated mediastinal/hilar mass. Hilar and/or mediastinal adenopathy are also commonly seen. Calcification within the mediastinum or hila can be seen in up to 86% of patients [13]. Bronchial obstruction can result in pulmonary infiltrates due to atelectasis or infection. Pulmonary venous obstruction manifests with localized pulmonary venous hypertension: peribronchial cuffing, septal thickening, and localized edema [13]. Vascular compression can result in infarction which can also produce peripheral wedge-shaped radiographic opacities. The presence of a dilated left superior intercostal vein (aortic nipple) can occur in association with superior vena caval obstruction. The extent of mediastinal involvement is frequently underestimated on the CXR [13].
CT: On CT, calcification (stippled or dense) of the mediastinal mass/adenopathy is common and is seen in up to 85% of cases (cakcification is typically absent in the diffuse infiltrative form [16]). Other CT findings include an infiltrative hilar/mediastinal mass, tracheobronchial narrowing, pulmonary vessel entrapment, SVC obstruction, and pulmonary infiltrates (due to bronchial obstruction with atelectasis, or pulmonary infarction due to vascular entrapment). Differential considerations include infiltrative malignancy (lung cancer, lymphoma, or mediastinal desmoid tumor).
MR: T1 images typically demonstrate a heterogeneous, infiltrating
intermediate signal mass on T1 images [13,14]. The T2 signal
appearance is more variable- with both regions of increased and
decreased signal [13]. Heterogeneous enhancement of the mass can
be seen following the administration of gadolinium [13]. Foci of
relative hypointensity may be seen on both T1 and T2 images caused
by calcifications or hypocellular collagenous scar [14].
Radionuclide studies are able to show abnormalities in perfusion
or ventilation secondary to vascular or airway narrowing. In one
reported case of FDG PET imaging, fibrosing mediastinitis appeared
predominantly as a hypometabolic mass which contained foci of
increased metabolic activity [13].
PET: There is variable degrees of FDG avidity which is likely
related to varying degrees of inflammation [16].
REFERENCES:
(1) Semin Roentgenol 1996; Conces DJ. Histoplasmosis. 31(1), 14-27 (No abstract available)
(2) Radiol Clin North Am 1994; High-resolution computed tomography in acute diffuse lung disease in the immunocompromised patient. 32(4), 731-744
(3) Medicine 1988; Loyd JE, et al. Mediastinal fibrosis complicating histoplasmosis. 67 (5): 295-310
(4) Chest 1994; Sherrick AD, et al. The radiographic findings of fibrosing mediastinitis. 106: 484-489
(5) AJR 1984; Farmer DW, et al. Calcific fibrosing mediastinitis: Demonstration of pulmonar vascular obstruction by magnetic resonance imaging. 143: 1189-1191 (No abstract available)
(6) AJR 1983; Weinstein JB, et al. CT of fibrosing mediastinitis: Findings and their utility. 141: 247-251
(7) J Thorac Cardiovasc Surg 1977; Dye TE, et al. Sclerosing mediastinitis with occlusion of pulmonary veins. 74 (1): 137-141
(8) Chest 1990; Dunn EJ, et al. Surgical implications of sclerosing mediastinitis. A report of six cases and review of the literature. 97: 338-346
(9) Mayo Clin Proc 1993; Espinosa RE, et al. Idiopathic pulmonary hilar fibrosis: An unusual cause of pulmonary hypertension. 68: 778-782
(10) Radiologic Clinics of North America 1997; McGuinness G. Changing trends in the pulmonary manifestations of AIDS. 35 (5): 1029-1082
(11) J Thorac Imag 1999; Conces DJ. Endemic fungal pneumonia in immunocompromised patients. 14: 1-8
(12) Society of Thoracic Radiology Annual Meeting 2000 Course Syllabus; Galvin JR. Histoplasmosis: The spectrum of disease. 81-82
(13) Radiographics 2001; Rossi SE, et al. From the archives of
the AFIP: Fibrosing mediastinitis. 21: 737-757
(14) AJR 2012; McNeeley MF, et al. Imaging of granulomatous
fibrosing mediastinitis. 319-327
(15) Radiographics 2016; Bachler P, et al. Multimodality imaging
of liver infections: differential diagnosis and potential
pitfalls. 36: 1001-1023
(16) Radiographics 2019; Garrana SH, et al. Multimodality imaging
of focal and diffuse fibrosing mediastinitis. 39: 651-667
(17) Radiographics 2021; Kunin JR, et al. Thoracic endemic fungi
in the United States: importance of patient location. 41: 380-398